Trochleoplasty
Dr. Garcia demonstrates his trochleoplasty technique
Trochleoplasty: A Comprehensive Overview
Trochleoplasty is a specialized surgical procedure designed to address trochlear dysplasia and associated patellar instability. This condition often leads to recurrent dislocations of the patella, significantly impacting knee function and quality of life. Trochleoplasty is particularly beneficial in revision surgeries where previous interventions have failed to correct the underlying anatomical abnormalities. This section provides an in-depth look at the background, indications, surgical procedure, risks, outcomes, and conclusions related to Trochleoplasty.
Background
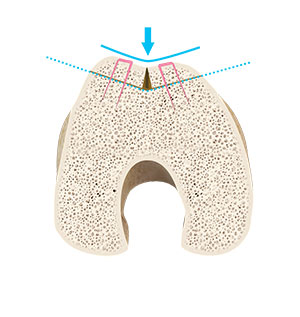
The trochlea is a groove at the lower end of the femur that accommodates the patella (kneecap) and guides its movement during knee flexion and extension. Trochlear dysplasia is a congenital condition where this groove is malformed, typically shallower than normal, resulting in poor engagement of the patella within the trochlea. This anatomical irregularity predisposes individuals to patellar instability, manifesting as frequent dislocations or subluxations (partial dislocations) of the patella.
Patellar instability is a debilitating condition, often associated with pain, swelling, and compromised knee function. When conservative treatments and less invasive surgical options fail to provide relief, Trochleoplasty becomes a viable solution. The goal of this procedure is to reshape the trochlea to create a more normal groove that can better stabilize the patella.
Indications
Trochleoplasty is indicated in several scenarios, primarily revolving around patellar instability and trochlear dysplasia. Key indications include:
- Recurrent Patellar Dislocations: Patients experiencing multiple dislocations despite non-surgical interventions.
- Trochlear Dysplasia: Confirmed radiographically, with a notably shallow or flat trochlear groove.
- Failed Previous Surgeries: Individuals who have undergone prior surgeries such as lateral release, medial patellofemoral ligament (MPFL) reconstruction, or osteotomies without satisfactory resolution of instability.
- Severe Symptoms: Persistent pain, swelling, and functional limitations impacting daily activities and sports participation.
Trochleoplasty
The Surgery
Trochleoplasty is a complex procedure typically performed by experienced orthopedic surgeons specializing in knee disorders. The surgery involves several critical steps:
- Preoperative Planning: Detailed imaging studies, including X-rays, MRI, and CT scans, are conducted to assess the extent of trochlear dysplasia and plan the surgical approach.
- Incision and Exposure: An incision is made over the knee to expose the trochlear groove. The patella is moved aside to provide clear access to the trochlea.
- Reshaping the Trochlea: Using specialized instruments, the surgeon removes bone from the femur to deepen the trochlear groove. This step may involve techniques like the Bereiter Trochleoplasty or Dejour Trochleoplasty, tailored to the specific anatomical needs of the patient.
- Stabilizing the Patella: Additional procedures, such as MPFL reconstruction or tibial tuberosity transfer, may be performed concurrently to further enhance patellar stability.
- Closure: Once the reshaping is complete, the patella is repositioned, and the incision is closed using sutures or staples.
Risks
As with any surgical intervention, Trochleoplasty carries inherent risks and potential complications. These include:
- Infection: Postoperative infections, though uncommon, can occur and may require antibiotics or additional surgery.
- Bleeding and Hematoma: Excessive bleeding during or after the procedure can lead to hematoma formation.
- Neurovascular Injury: Damage to surrounding nerves and blood vessels, although rare, is a potential risk.
- Joint Stiffness: Postoperative stiffness may necessitate physical therapy or further surgical intervention.
- Nonunion or Malunion: Incomplete or improper healing of the reshaped trochlea can affect outcomes and may require revision surgery.
- Residual Instability: Despite surgery, some patients may continue to experience patellar instability, necessitating additional treatments.
Outcomes
The success of Trochleoplasty is measured through various parameters, including knee stability, pain relief, functional improvement, and patient satisfaction. Clinical studies and patient reports generally indicate favorable outcomes:
- Knee Stability: Trochleoplasty effectively stabilizes the patella, significantly reducing the incidence of dislocations and subluxations. Post-surgery, patients typically report a marked improvement in knee stability.
- Pain Relief: By addressing the underlying anatomical issues, Trochleoplasty alleviates pain associated with patellar instability and trochlear dysplasia.
- Functional Improvement: Patients often experience enhanced knee function, allowing them to resume daily activities and sports with greater confidence and less discomfort.
- Patient Satisfaction: High levels of patient satisfaction are commonly reported, attributed to the significant improvements in stability, pain, and overall knee function.
Conclusion
Trochleoplasty represents a crucial advancement in the surgical management of trochlear dysplasia and patellar instability. This procedure offers a reliable solution for patients who have not found relief through conservative measures or previous surgeries. By reshaping the trochlear groove, Trochleoplasty addresses the root cause of instability, providing lasting improvements in knee function and quality of life.
However, it is essential to recognize that Trochleoplasty is a complex procedure with potential risks and complications. Success depends on careful patient selection, meticulous surgical technique, and comprehensive postoperative care. Patients considering Trochleoplasty should engage in thorough discussions with their orthopedic surgeon to understand the benefits, risks, and expected outcomes.
As advancements in surgical techniques and postoperative rehabilitation continue to evolve, the future of Trochleoplasty looks promising, offering renewed hope for individuals suffering from debilitating patellar instability and trochlear dysplasia. With the right approach, Trochleoplasty can restore stability, function, and confidence, enabling patients to return to their active lifestyles with minimal limitations.